There are two fundamental tenets of MSK imaging:
Protocols:Therefore, basic MR protocols include anatomy defining sequences such as: T1, GRE's and Proton Density (PD or 1st echo T2) and fluid sensitive sequences such as Inversion Recovery (IR) and PD fat saturation, although there is overlap between them. T1 post-intrarticular and post-intravenous contrast are also used, for definition of anatomy and detection of pathology respectively.
Equipment:All MR protocols assume 1.5T or greater and appropriate phased array surface coils where possible.
Positioning:The positioning of the patient must also be taken into account in certain instances to better align the anatomical structure being studied.
Sequences Defining Anatomy
What attributes make a sequence good for defining anatomy?
- Proper balance between signal to noise ratio (SNR) and resolution
- Optimizes visualization of inherent tissue contrast
- Fast acquisitions (reduces motion artifact)
- Orientation along anatomical structure being studied

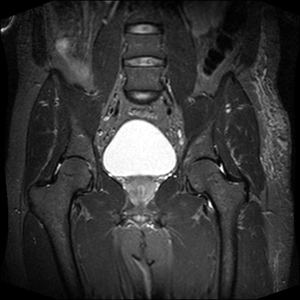
Note how the inherent T1 tissue contrast is optimized by the sequence, and how the bladder is low signal.
Bright On T1:
- Fat
- Gadolinium
- (And occasionally encountered in musculoskeletal imaging: proteinaceous fluid and subacute hemorrhage

Confusing terminology:
The term Proton Density is actually an inaccurate term, as it implies that the only contrast mechanism of the image is based on differences in proton density. In fact, contrast is predominantly derived from intermediate weighting between T1 and T2. Most, so called PD sequences have TRs that are too short to completely eliminate T1 contrast and TEs that are too long to completely eliminate T2 contrast. Intermediate-weighted is a more accurate term, as is well depicted by the bladder in this image.
The PD sequence is also often the 1st echo of a dual-echo T2 sequence.
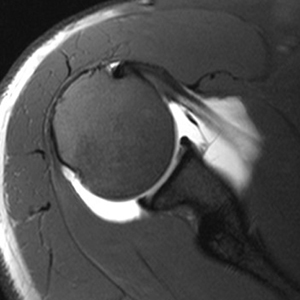
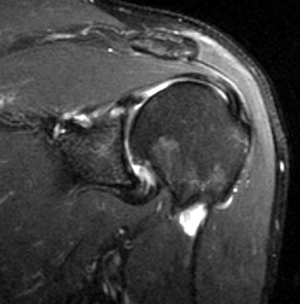
T1 fat suppressed, intra-articular gadolinium sequences result in a high signal to noise ratio and joint distension. This allows visualization of structures that are normally too crowded to fully visualize.
Note: the subcutaneous fat is bright due to inhomogeneous fat suppression, a very common artifact.
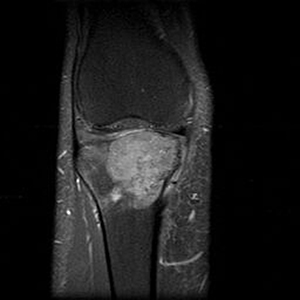
Gradient echo techniques are particularly effective in assessing cartilage due to their ability to obtain thin sections. Fat suppression may be used with gradient echo and eliminates chemical shift artifact that can distort the cartilage-bone interface. In addition, fat suppression narrows the gray scale range, providing greater contrast.
Sequences detecting abnormal fluid/enhancement:
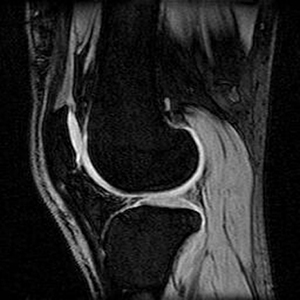
- PD/T2 fat suppressed and IR sequences are all sensitive to the detection of fluid, although they obtain these results by different mechanisms. PD gives higher SNR, while T2 and IR are more sensitive to fluid.
- T1 post gadolinium fat suppressed (T1 PGfs) sequences are more commonly used in MSK MR for additional evaluation of a lesion rather than the initial detection of that lesion.
- *Keep in mind that chronic injuries/changes may not have edema, and that detection of chronic pathology may solely depend on detection of aberrations in anatomy.
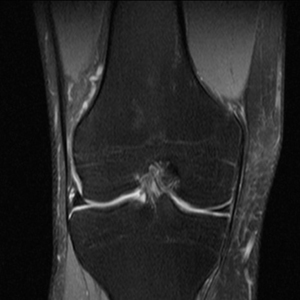
The conspicuity of fluid is maximized while maintaining a high SNR. Fat suppression narrows the gray scale range, allowing for increased contrast.
Note how the T1 signal intensity of fat has been nulled, resulting in decreased SNR but distinct fluid, as is well depicted by the bladder in this image.
T2 fat suppressed sequences allow detection of fluid while avoiding magic angle artifact that can occur with short TE sequences such as PD or IR.
T1 fat suppressed IV gadolinium sequences, are used to help detect small lesions/recurrence, or to further define a lesion's properties such as vascularity, inflammation, soft tissue involvement, relation to neurovascular bundles, etc.
